Start with a concrete plan: map location and sites to align volume with processing timelines. This general approach clarifies identity and problem areas in developing settings and highlights the disorders that affect most patients with linked conditions. The framework surveys sites to capture data across the workflow from start to release, and it keeps manual inputs and late updates visible to flag bottlenecks. It also emphasizes that any adjustment to design requires cross-functional input to avoid misalignment with carriers and technology constraints.
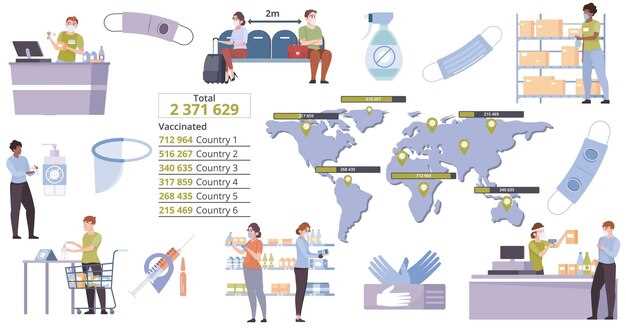
The triad of logistics challenges begins with site readiness and the design of patient access points. Ensure sites can receive material, perform processing, and hand off to carriers that maintain strict temperature and tracking controls. A second pillar focuses on technology for inventory and traceability, linked to patient identity to prevent misassignment at late handoffs. The third pillar covers data flow and manual reconciliation across location networks, so start of manufacturing aligns with forecasted volume for the most sites and prioritizes high-value patients. location checks ensure alignment between samples and records at every handoff.
In developing networks, implement a practical design to quantify the volume at each site and simulate late-stage handoffs to carriers so that processing capacity matches demand without compromising identity. Rely on technology stacks that support rapid processing data entry and manual reconciliation when routine scans fail. Prioritize high-value patients and most urgent cases by location, ensuring the triad remains stable across shifting demand and regional disorders.
Apheresis Scheduling for Faster Patient Access
Centralize scheduling across hospital networks and university-affiliated centers to lock in appointment times and date blocks for therapeutic apheresis, reducing patient wait and transfer steps. Coordinate with suppliers to confirm single-use kits and consumables days in advance, preventing last-minute backorders. Use a simple design that can be easily transitioned from manual workflows to automated tools while aligning with patientsregulatory guidelines.
Key actions to accelerate access
Establish a centralized hub that coordinates times, date windows, and site readiness across country networks. Engage with hospital and university teams to pre-confirm patient eligibility and essential services, minimizing delays when they arrive. Maintain a live inventory log with suppliers to confirm stock levels for single-use components and necessary consumables at each facility. Maintain a list of needed consumables and equipment to prevent gaps.
Operational design and site types
Structure the workflow around location types: hospital wards, a dedicated facility, and mobile collection units where applicable. Leverage traditional procedures alongside modern technologies to harmonize calendars across sites, preventing double-bookings. The shared calendar should handle rescheduling easily, with clear ownership for each date window and time slot, and with safeguards that protect patient data and patientsregulatory requirements.
Risk management, staff support, and innovation: implement readiness checks to reduce failed starts, verify patient identity and anticoagulation needs, and have backup locations to handle peak demand. Use a mix of manual steps and automation to keep processes resilient, while documenting all changes to them and ensuring staff are trained to adapt quickly. This approach supports hospital teams, end-to-end services, and innovation in scheduling practice. Address the critical things–kit availability, staffing, and data integrity–to shorten access times and improve patient flow across locations.
Metrics and governance: track country-wide time-to-appointment metrics, actual start times, date accuracy, and slot utilization. Maintain records of kit types and suppliers used, linked to each facility and location, to optimize future blocks. Define an innovation loop to pilot new scheduling algorithms or technologies and scale successful changes across sites.
Manufacturing Throughput and QC Turnaround
Adopt parallel QC lanes across centers to shorten turnaround to 24-48 hours, boosting throughput and speeding patient access. Start by standardizing release criteria, looking at modular, single-use workstreams that minimize changeover and reduce hands-on time, allowing teams to push more work between shifts.
Establish two QC tracks: on-floor in-process checks and a centralized finished-product QC run, with predefined acceptance criteria that allow release within a single shift. Include well-defined touch points and data hooks to ensure results align with release decisions.
Timing and schedule are core levers: implement a rolling schedule that ties start times to outbound shipments, map those windows, and ensure sent times are tracked across centers. This coordination reduces idle time and improves cycle predictability.
Invest in automation to reduce hands-on handling and minimize error-prone manual steps, looking at modular, closed systems and robotic sample preparation. Among the gains are shorter cycles, lower labor cost, and more consistent process performance globally.
Emerging centers require common data standards; pagliarulo notes that cross-site alignment yields the biggest business gains, among those needs is standardized data exchange and clear ownership; yescarta teams show that integrated scheduling and QC collaboration cut rework and latency across networks.
Cost discipline: execute a staged capex plan for modular cells and flexible workcells, balancing upfront investments with ongoing savings from faster throughput. Use nitrogen management to protect sample integrity during handling and storage, reducing deterioration risks and waste.
Globally, synchronize metrics, sharing best practices across centers with a centralized dashboard. Among those metrics: batch size, time to result, disposition rate, and deterioration incidence; they provide early signals so teams can act quickly. This enables rapid corrective actions and continuous improvement.
Cold-Chain Management: Ensuring Viable Cells from Collection to Infusion
Implement a validated, end-to-end cold-chain protocol with continuous temperature monitoring and real-time alerts from collection to infusion. thats central to maintaining viable cells for patient outcomes and to avoid waste; for car-t products, dwell times on transport must be minimized and handling procedures standardized.
Key elements include validated packaging, data-loggers with alarms, and robust transport modes. Storage uses liquid nitrogen at -196°C; short-stage transport can use dry ice at -78.5°C, but product-specific validated ranges must be followed; predicted viability windows depend on product type and were established in the master procedures. vineti-approved carriers and marken policies support integration with hospitals and pharmaceutical partners; this reduces risk and improves benefits, while ensuring destination viability and regulatory compliance. excursions might occur during transit, but alarms and corrective actions mitigate impact.
Regulatory alignment: policies require full traceability from collection to the destination; patientsregulatory expectations require transparent documentation and consistent procedures; to justify the investment, quantify risk reduction, patient access, and market expansion for therapeutic treatment. This approach requires disciplined governance and ongoing verification. The integration of providers and hospitals with commercial pharmaceutical partners supports market growth while maintaining safety and effectiveness.
| Phase | Risks and Critical Controls | Metriky |
|---|---|---|
| Collection and Processing | Temperature excursions, labeling mismatch, handling errors; Controls: validated packaging, dual-labeling, real-time data loggers; ensure TTIs and clear procedures | % excursions >2°C, time outside validated window, audit-trail completeness |
| Cryopreservation and Storage | Power loss, freezer LN2 failure, supply disruption | Uptime percentage, temperature stability (±1°C), LN2 level checks |
| Transport to Destination | Transit delays, temperature shifts, improper courier handling | Average transit time, excursion rate, TTIs triggered |
| Infusion Preparation | Thaw shock, contamination during handling, equipment errors | Viability post-thaw, recovery yield, time from thaw to infusion |
Inventory Strategy: Balancing Autologous vs Allogeneic CAR-T Options
Recommendation: Implement a dual-track inventory policy that keeps autologous components at regional infusion centers while maintaining a centralized pool of allogeneic material to enable infused doses within 24–72 hours after lymphodepletion, ensuring patient access and alignment with market demand.
- Demand forecasting by country and market: deploy a single source of truth that translates referrals and indications into site-level targets; adjust weekly based on new research and observed uptake; referred data inform replenishment to ensure appropriate supply across sites.
- Inventory segmentation: maintain separate reservoirs for components and finished products; enforce distinct expiry criteria and discard rules; many items are perishable and subject to deterioration without timely utilization.
- Storage and handling: use nitrogen-blanketed cryopreservation and strict temperature controls; maintain an interface between the storage system and ERP/LIMS to flag excursions; adding preventive maintenance and audit trails in sops.
- Production cadence and technologies: autologous workflows demand modified manufacturing runs on demand, while allogeneic pipelines rely on innovative, off-the-shelf technologies; align both streams to an integrated schedule to minimize lead times and ensure timely infusion.
- Quality control and testing: implement a robust sampling plan (samples) for pre-infusion verification, including receptor expression and potency assays; ensure acceptance criteria are appropriate and aligned with regulatory expectations; referred to by regulatory guidelines and include these checks in sops.
- Supply risk and interface governance: develop a resilient logistics interface among suppliers, manufacturing, and clinical sites; monitor market volatility and regulatory changes; continue to refine risk controls with research outputs and real-world data.
- Lifecycle optimization and continuous improvement: leverage country-specific feedback and ongoing research to adjust stock targets; innovative analytics found that dual-track inventory improves access and reduces patient wait times; many programs continue to evolve, incorporating new samples and added modalities as they become available; this approach continues to adapt as new findings emerge.
Regulatory Readiness and Real-Time Quality Surveillance
Establish a regulatory-ready, real-time QC surveillance platform that triggers CAPA workflows within hours of any deviation, ensuring end-to-end traceability from lot release to patient treatment date. Alerts are routed to quality, manufacturing, regulatory, and clinical teams; operational drills test them and remind them of response time targets.
Use a modular data model that ingests manufacturing results, release judgments, quality records, pharmacovigilance signals, and post-infusion outcomes, including modified car-ts products and allogeneic formats, which informs risk analyses and improvement actions.
Map data fields to regulatory expectations across jurisdictions, document validation evidence for both autologous-like and allogeneic pathways, and maintain a single source of truth to reduce the problem of late rework and date drift. For most authorities, alignment also supports faster approvals and clearer post-market surveillance, reducing the required review cycles.
Novartis demonstrates a centralized, digitized workflow; markens dashboards illustrate real-time analytics on yields, defects, and safety; these exemplars show what contributes to improved costs and patient outcomes.
Training investments must cover operators, QA staff, and clinical teams; allocate hours for initial onboarding and quarterly refreshers, and reserve resources for exception investigations. thats essential to ensure the system continues to support treatment continuity and compliance, even as product complexity grows.
Data governance and real-time monitoring
Define data ownership, access controls, and end-to-end audit trails; implement standardized data dictionaries and KPIs for completeness, timeliness, and accuracy to satisfy regulators and internal stakeholders.
Ensure interoperability with suppliers, central laboratories, and clinical partners; document version history for all changes to processes, materials, and assays to prevent misalignment and delays.
Workforce readiness and cost management
Develop a training calendar for operations, quality, and regulatory teams; plan for dedicated resources, track training hours, and monitor costs against expected benefits; manage updates as advances in car-ts modalities emerge.

 CAR-T Therapies – Three Supply Chain Considerations">
CAR-T Therapies – Three Supply Chain Considerations">
